AMS eChanges Volume 2023:02 | 27 February 2023
|
||||||
|
Hello Magdalena,
Our eChanges will contain, as available, new information sheets, case studies, news about new medications in the management of menopause and updates on conferences and meetings.
The latest edition of eChanges is also available when logged in to the AMS Members area of the website here for easy desktop or tablet viewing. Inside this issue
AMS News February 2023
- President's Report - IMS World Congress on Menopause in Melbourne 2024 - Improving my practice with online mental health resources – a GP reflects - AMS Advocacy Campaign and Menopause Survey for Women - Get on board! - 26th AMS Congress, Queenstown, New Zealand, 1-3 September 2023 News from Around the World - Impact of hormone therapy on the bone density of women with premature ovarian insufficiency - Menopausal vasomotor symptoms and white matter hyperintensities in midlife women - Our Menopause World February 2023 - European Menopause and Andropause Society (EMAS) Newsletter AMS News February 2023President's Report Dear AMS Members, Many AMS members are clinicians who treat women with early or premature menopause or see the consequences of inadequate clinical care. Early menopause is the loss of ovarian function under the age of 44 and affects up to 12% of women. Premature menopause, also called premature ovarian insufficiency (POI), is the loss of ovarian function under age 40, and is experienced by up to 4% of women globally.(1) Early and premature menopause can be spontaneous or can be caused by medical treatments such as chemotherapy, radiotherapy or surgical removal of the ovaries. POI should be considered when a woman under 40 presents with oligo/amenorrhoea. Unfortunately, the diagnosis is sometimes delayed as women or their clinicians may not consider POI as a cause of oligo/amenorrhoea, preferring alternative explanations such as post-pill amenorrhoea or polycystic ovarian syndrome. Delayed diagnosis can lead to missed opportunities in fertility, bone health, sexual health, cardiovascular health and psychosocial support for women. A diagnosis of POI can be unexpected and devastating and appropriate support should be offered. Women need a comprehensive assessment including evaluation for a cause (Figure 1) and for management of both short- and long-term health. Referral to an appropriate specialist is recommended. A suggested approach to the management of women with POI is summarised in this algorithm (Figure 2). For some women loss of fertility is the primary concern.(2) Sexual health and management of genitourinary symptoms should be addressed. Assessment of bone health is important, along with reducing modifiable risk factors for osteoporosis, and optimising calcium, vitamin D and exercise. Bone densitometry is MBS reimbursed in Australia for women with hypogonadism aged under 45 years. Hormone replacement therapy is recommended for women without contraindications, for maintenance of bone health. Hormone therapy containing at least 2 mg oral estradiol or equivalent is needed to maintain bone density.(3) Cardiovascular disease risk is elevated in women with POI. Assessment and management of risk factors and promotion of healthy lifestyle is very important. Hormone therapy may reduce risk.(4) Women with POI need high quality information to guide them. There are now excellent resources available to women with early menopause including Askearlymenopause, a freely available app giving reliable information (Figure 3). Australian general practitioners are reminded that patients with POI are eligible for Chronic Disease Management Plan item numbers under Medicare. Many women will benefit from a multidisciplinary team approach including allied health practitioners such as exercise physiologists, psychologists, dieticians and physiotherapists. Clinical Associate Professor Amanda Vincent, a Past President of AMS and a current Board member of the International Menopause Society, leads a research and education program at Monash University. Her team have developed the algorithms reproduced here, and a range of other resources. Amanda is part of an international group updating the 2016 European Society for Human Reproduction and Embryology POI guideline,(4) expected to be ready next year. POI will also be part of the IMS World Congress on Menopause in Melbourne 2024 – so save the date! References
A PDF of Algorithm: Diagnosis/evaluation of premature ovarian insufficiency for personal use is available here 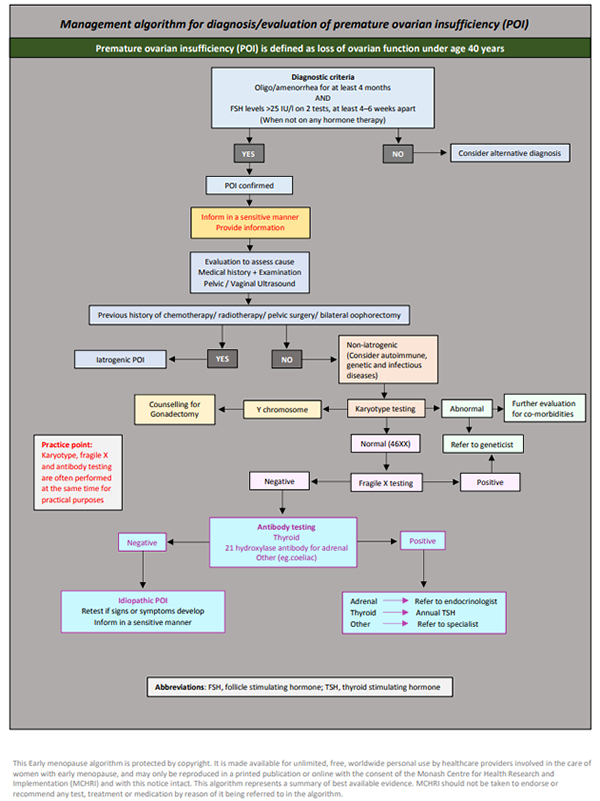 Reproduced with permission from Monash Centre for Health Research and Implementation (MCHRI), Monash University, Clayton, Victoria, Australia A PDF of Algorithm: Management of premature ovarian insufficiency for personal use is available here 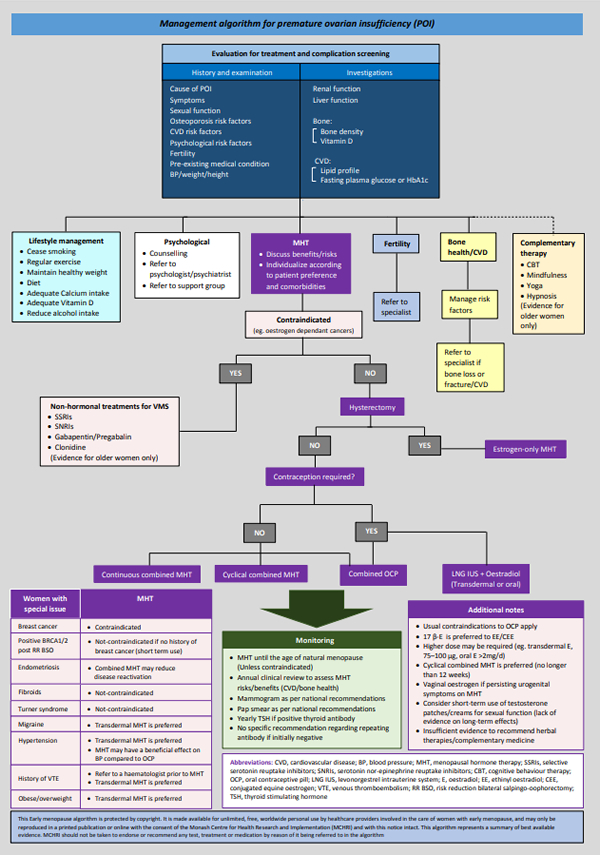 Reproduced with permission from Monash Centre for Health Research and Implementation (MCHRI), Monash University, Clayton, Victoria, Australia Yours sincerely, Dr Karen Magraith IMS World Congress on Menopause in Melbourne 2024Improving my practice with online mental health resources – a GP reflectsDr Carmel Reynolds I had planned to spend my summer break reading useful books that are available for women trying to manage menopausal symptoms. I have a collection and thought I would: 1) make my own notes about who the books would help; 2) appraise the quality of the information; and 3) have them ready to lend once I got back to work. The books are very new and still in a neat pile on my bedside table. The reality is, at the end of 2022, I was really tired and I wanted to read books that were fun, light-hearted and didn’t require any great academic appraisal – and did not mention COVID. Instead, I decided to think about how GPs and other non-GP specialists can better use and be assisted by books, online resources and apps. Much has been documented in GP literature about high rates of burnout and dissatisfaction with increasing workloads combined with fewer resources and less money. GPs are retiring, changing to other subspeciality roles, reducing hours and we have not been able to fill training positions. Fewer medical graduates are interested in pursuing a career in General Practice.(1) Popular media outlets seem to want to brand us as greedy doctors, patients cannot get appointments and people can’t afford appointments. From my perspective, I want a system that is fit for purpose and, yes, I do want to be paid for the work I do. But what I really want is to be able to access services for my patients. This is my job. I care about people and I want to help, but I know so many people are barely getting by week to week and more than are few are sinking further into debt. I can’t do my job well if patients cannot access the care they need. Despite that doom and gloom, I really like my job. I like being a GP. I have a unique window into people’s lives and can offer comprehensive “holistic” and intergenerational care. I am sure many, if not most GPs, feel the same. My style is mostly slow medicine. I assist a cohort that is female predominant, too often with a history of not being heard and with high rates of mental health concerns. Again, I am sure many of you reading this are in the same boat. I would like item numbers that reward this work, without feeling like we cannot bill them for fear of audit. Menopause consults are often longer and incorporate symptom management, chronic disease prevention, early detection of cancer and mood symptoms. Yet, there is no adequate single item number that reflects the work involved. And it is known that many of us often under-bill.(2) Why am I writing about this in eChanges? I want healthcare reform that acknowledges this work and makes it easier to build multi-disciplinary teams that people can afford to access. To say I felt frustrated when the government reduced funding to psychological therapies for 2023 by half is an understatement. I acknowledge but won’t be able to address the inequities of access to these services that have always existed and remain – not to mention the long wait times faced by those who can afford to access psychological therapy. We know that mood symptoms are common in perimenopause and that the rates are higher in those with a previous depressive episode or history of hormone-related mood disorder. Perimenopausal depression and anxiety present differently to other mood disorders and using a menopause-specific assessment tool such as Meno D can help in diagnosis. Consideration of hormonal therapy (MHT), antidepressant medication and psychological therapies all need consideration.(3) We know that Cognitive Behaviour Therapy can help manage mood symptoms, hot flushes and sleep issues.(4) How do we assist access to these therapies while we have reductions in funding, increasing gaps and limited availability of practitioners? Invariably much of this falls back on the GP to manage, with a reduction in multidisciplinary care. I used my holiday to make a mental to-do list. One of the items on my list was to collate a list of e-health resources and find recommendations for books from trusted sources. There is evidence to suggest that e-health resources can be effective in the management of mild- moderate anxiety and depression. They offer convenience, are often low or no cost and are cost effective and time efficient.(5) Menopause is trendy right now and there is a lot of good information out there, but unfortunately a lot of misinformation is also available. I think it is helpful for us to have some knowledge of trends and be able to suggest sites that are evidence based. Below is a short list of my go-to mental health resources and I hope this is helpful to you. Some resources, such as “This Way Up”, allow practitioners to register and refer, waiving the patient fee and keeping us informed of their progress. I continually find new resources and information and it will take a time commitment from me to get a better understanding of what they can offer. I also have favourite social media sites specifically for menopause, but I won’t include all of those here. I follow the Australasian Menopause Society (AMS) on the usual socials (AMS is on twitter, Facebook, LinkedIn and Instagram) and follow our President (@KarenMagraith) on twitter. I share the information on the AMS website with colleagues and consumers alike – we have excellent resources. I will read that pile of books I mentioned – perhaps on the plane on my way to Queenstown for the AMS 2023 Congress. Online mental health resources
References
Article available online here AMS Advocacy Campaign and Menopause Survey for Women - Get on board!The AMS advocacy campaign to raise awareness of menopause and direct health professionals and consumers to evidence-based information and resources on menopause and midlife women’s health is underway. This advocacy campaign ties in with the upcoming Parliamentary Round Table discussion entitled “Menopause Matters” on 7 March 2023 which is being hosted by AMS, where we will advocate for health professional education and community awareness about menopause. AMS is running a social media campaign #EmbracetheChange and we encourage you and your patients to engage and cross-promote on platforms such as Facebook, LinkedIn, Twitter and Instagram and also by tagging us with #AMSmenopause. AMS is also surveying consumers experience of menopause to collect some quick, easy data that we can highlight to government. It is not intended to be a representative sample, but has been designed with mostly closed questions so we can analyse quickly. The survey can be found here or via the QR Code and we encourage you to pass it on to anyone that you know who is peri- or post-menopausal.
26th AMS Congress, Queenstown, New Zealand, 1-3 September 2023 The AMS is pleased to advise that the 26th AMS Congress will be held at The Millennium Hotel, Queenstown, New Zealand from 1-3 September 2023. The theme of the Congress is “Remarkable reflections on midlife and menopause”. Dr Ashley Makepeace is Chair of the Scientific Committee and will be sure to put together an up-to-date and stimulating scientific program. Dr Sylvia Rosevear is Chair of the Local Organising Committee and is looking forward to welcoming delegates to Queenstown to experience the beauty and adventure of this amazing destination. So please add the dates 1-3 September 2023 in your diaries and keep up to date about the Congress at www.amscongress.com.au News from Around the WorldImpact of hormone therapy on the bone density of women with premature ovarian insufficiencyIMS Live: 31 January 2023 SummaryWomen with premature ovarian insufficiency (POI) are exposed to a long period of estrogenic deficiency, which potentially brings higher health risks, especially regarding bone health. Recently Costa et al. [1] performed a systematic review of the literature to evaluate the effect of hormone therapy (HT) on bone mineral density (BMD) in women with POI. They performed a search in MEDLINE and EMBASE databases up to September 2021 and included studies that analyzed women with spontaneous idiopathic POI treated with HT, to whom BMD was evaluated. Analysis of risk of bias of the selected studies was also performed. The authors found 335 articles and selected 16 studies according to the inclusion criteria. Most of the studies revealed lower bone density in both the femoral neck and lumbar spine in women with POI compared with healthy women. Bone mass had the tendency to remain stable in women treated with estrogen + progestin therapy; however, in those already with bone mass loss, the therapy - in the doses most frequently used - was not able to revert the loss. Higher estrogenic doses seemed to have a positive impact on BMD, as did combined oral contraceptives used continuously. In addition, the interruption of HT for longer than one year was associated with significant bone loss. The authors conclude that although HT brings clear benefits, further studies are needed to establish its long-term effects, as well as doses and formulations with better protective effects on the bone mass of women with POI. CommentaryThis is a useful systematic review [1] of the currently available data concerning POI and the impact of various HT regimens including menopause hormone therapy (MHT) and the combined oral contraceptive pill (COC) on BMD. Despite the stated limitations, it illustrates several issues which are important for clinical practice; these are:
Unfortunately, long-term prediction of POI using biomarkers such as anti-mullerian hormone remains problematic [2,3]. We must therefore combine clinical acumen with public health information, for example, menstrual irregularities should be reported early to primary healthcare providers. Toolkits for primary care physicians can also be of assistance in the early diagnosis and efficient management of POI [4]. Menopausal vasomotor symptoms and white matter hyperintensities in midlife womenIMS Live: 13 February 2023 SummaryRecently, Thurston et al. [1] investigated whether vasomotor symptoms (VMS), when rigorously assessed using physiologic measures, were associated among midlife women with greater white matter hyperintensity volume (WMHV). The authors considered a range of potential explanatory factors in these associations and explored whether VMS were associated with the spatial distribution of WMHV. For this, women aged 45-67 (n=226) who were free of hormone therapy underwent 24 hours of physiologic VMS monitoring (sternal skin conductance), actigraphy assessment of sleep, physical measures, phlebotomy, and 3 Tesla neuroimaging. Associations between VMS (24-hour, wake, and sleep VMS, with wake and sleep intervals defined by actigraphy) and whole brain WMHV were analyzed in linear regression models adjusted for age, race, education, smoking, body mass index, blood pressure, insulin resistance, and lipids. Secondary models considered WMHV in specific brain regions (deep, periventricular, frontal, temporal, parietal, occipital) and additional covariates including sleep. The investigators found that physiologically-assessed VMS were associated with greater whole brain WMHV in multivariable models, with the strongest significant associations observed for sleep VMS [24-hour VMS, wake VMS, sleep VMS]. Associations were not accounted for by additional covariates including actigraphy-assessed sleep (wake after sleep onset). When considering the spatial distribution of WMHV, sleep VMS were associated with both deep, periventricular and frontal lobe WMHV. The authors conclude that VMS, particularly those occurring during sleep, were associated with greater WMHV. In addition, they recommend the crucial need of finding female-specific midlife markers of poor brain health later in life in order to identify women who warrant early intervention and prevention. VMS have the potential to serve as this female-specific midlife marker of brain health in women. CommentaryVMS are commonly regarded just as annoying and uncomfortable side effects of ovarian failure, which may either be temporary and wane within up to several years in the postmenopause, or can be successfully treated by menopausal hormone therapy, but having no otherwise health significance. Contrarily, many recent studies showed that VMS are related to important clinical situations, and therefore the occurrence of VMS should raise attention to potential problems in various body systems. Accumulating evidence indicates that VMS are associated with cardiovascular health and with an increased risk for several chronic diseases, including the metabolic syndrome, obesity, type 2 diabetes mellitus, non-alcoholic fatty liver diseases, and osteoporosis in peri- and postmenopausal women [2]. White matter hyperintensities (WMHs) are brain white matter lesions that are hyperintense on fluid attenuated inversion recovery magnetic resonance imaging (FLAIR-MRI) scans. WMHs are commonly seen on brain MRIs in older people, but appear also in certain disease conditions, mainly in neurological and psychiatric disorders [3]. One of the underlying mechanisms is ischemia, expressed as small vessel disease. Larger WMH volumes have been associated with Alzheimer's disease (AD) and with cognitive decline [4]. So these are the facts: 1) the menopausal transition has been recognized as an important period for women's brain health; 2) VMS frequently occur from the early stage of menopause onward; and 3) the existence of WMHs points at a higher risk for cognitive decline. The present commented paper of Thurston et al. [1] tied all these parameters and investigated the association between VMS, monitored objectively by sternal skin conduction rather than according to women’s subjective report, and WMHs recorded by very accurate MRI scans. Study findings pointed at a clear association between VMS, especially if occurring during sleep [5], and greater whole brain WMH volume. Such results may indicate that VMS should be considered as a valuable early marker for future cognitive impairment. Understanding the scope of the VMS phenomenon clearly contradicts the previous commonly held belief of its irrelevance to major health issues in various body systems. Our Menopause World February 2023President’s Report Dear Friends and Colleagues, It is a great pleasure to communicate with you once again. It has been a busy start to the year for the International Menopause Society.
There was also much discussion about the organisational structure of the IMS going forward, with emphasis on the importance of the many “sub” committees which are an invaluable way of the IMS Executive and Board obtaining new information from our wider membership. New committees in development include Menopause Info, Young Professionals, Council of Affiliated Menopause Societies (CAMS) steering group and IMS Recommendations. We will be reaching out soon to a you, our members, to help populate these committees.
However, it was not accepted by the government that menopause should be a characteristic protected by law. There is still much work to be done, but I believe that much progress has been made, and some aspects could be adapted in other countries and regions of the world, with appropriate sensitivity to local political, cultural, religious and financial issues.
European Menopause and Andropause Society (EMAS) NewsletterAMS is an affiliate of EMAS. See a copy of the |
||||||
 |
||||||
| Copyright © 2023 Australasian Menopause Society Ltd. PO Box 280, Healesville VIC 3777 Tel: +61 3 5962 6241 | Email: ams@menopause.org.au |
||||||
|
Contact us | Unsubscribe |
||||||