Australia
Please note that Femoston-Conti 1/5 has been delisted from the PBS and is only available on private script from 1 December 2023. Patients who have been prescribed Femoston-Conti 1/5 before 1 December 2023 will be able to have it dispensed at the PBS listed price until 1 March 2024. We understand that the delisting is a commercial decision made by the sponsor. While private script prices fluctuate between pharmacies, Femoston-Conti 1/5 is currently being sold at a large pharmacy chain for $11.99 on a private script.
|
Product
|
Composition
|
Date of deletion
|
|
Climara 25
|
25mcg oestradiol transdermal patch
|
Deleted
|
|
Climara 50
|
50mcg oestradiol transdermal patch
|
15 Mar 2024
|
|
Climara 75
|
75mcg oestradiol transdermal patch
|
Deleted
|
|
Climara 100
|
100mcg oestradiol transdermal patch
|
Deleted
|
There are a number of MHTs that are currently unavailable. Please note that the TGA has approved some unregistered products for supply under Section 19A.
|
Product
|
Composition
|
Expected supply due
|
Section 19A Approved Equivalent
|
|
Estradot 25
|
25mcg oestradiol
|
26 Apr 2024
|
Estramon oestradiol 50mcg
|
|
Estradot 37.5
|
37.5mcg oestradiol
|
17 May 2024
|
Estramon oestradiol 37.5mcg
|
|
Estradot 50
|
50mcg oestradiol
|
26 Apr 2024
|
Estramon oestradiol 50mcg
|
|
Estradot 75
|
75mcg oestradiol
|
17 May 2024
|
Estramon oestradiol 75mcg
|
|
Estradot 100
|
100mcg oestradiol
|
17 May 2024
|
Estramon oestradiol 100mcg
|
|
Estraderm MX 25
|
25mcg oestradiol
|
Available
|
|
|
Estraderm MX 75
|
75mcg oestradiol
|
15 Mar 2024
|
|
|
Estraderm MX 100
|
100mcg oestradiol
|
Available
|
|
|
Estalis Sequi 50/140
|
50mcg 17β oestradiol/140mcg norethisterone acetate
|
Unavailable
|
|
|
Estalis Sequi 50/250
|
50mcg 17β oestradiol/250mcg norethisterone acetate
|
1 Mar 2024
|
|
|
Estalis Conti 50/140
|
50mcg 17β oestradiol/140mcg norethisterone acetate
|
Available
|
|
|
Estalis Conti 50/250
|
50mcg 17β oestradiol/250mcg norethisterone acetate
|
Available
|
|
The AMS Guide to MHT Doses (Australia only) provides a guideline to approximately equivalent doses of the different MHT/HRT products in Australia.
New Zealand
A list of patch availability is provided below.
|
Dose
|
Estradot
|
Viatris
|
Mylan
|
|
25mcg
|
Low supply
|
n/a
|
Unavailable
|
|
50mcg
|
Low supply
|
Unavailable
|
Unavailable
|
|
75mcg
|
Unavailable
|
Unavailable
|
Unavailable
|
|
100mcg
|
Unavailable
|
Available
|
Unavailable
|
More information can be found at here
The AMS Guide to MHT Doses (New Zealand only) provides a guideline to approximately equivalent doses of the different MHT/HRT products in New Zealand.







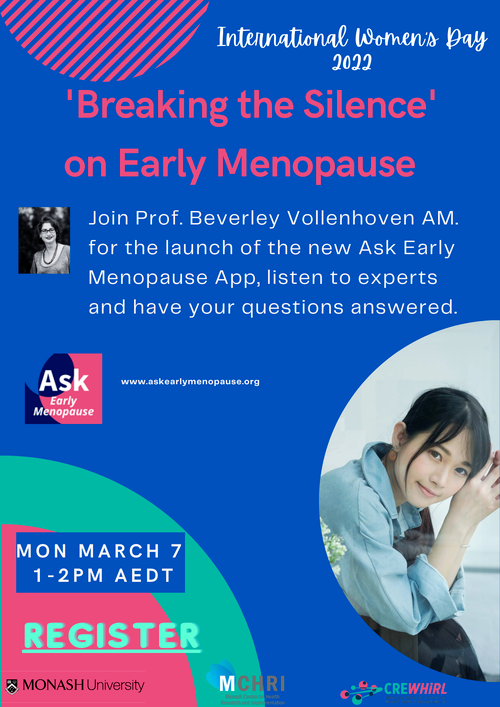 The theme of International Women’s Day for 2022 is ‘Breaking the bias’. Researchers at Monash Centre for Health Research and Implementation, Monash University, have chosen this day to ‘break the silence’ on early menopause, to launch their new evidenced based App for women Ask Early Menopause. Developed by women for women, and with multidisciplinary early menopause expert input, the App includes women’s stories, evidence-based information, animation and a personalised dashboard to help women manage early menopause and premature ovarian insufficiency. Development of the App was undertaken as part of the CRE in Women’s Health in Reproductive Life (
The theme of International Women’s Day for 2022 is ‘Breaking the bias’. Researchers at Monash Centre for Health Research and Implementation, Monash University, have chosen this day to ‘break the silence’ on early menopause, to launch their new evidenced based App for women Ask Early Menopause. Developed by women for women, and with multidisciplinary early menopause expert input, the App includes women’s stories, evidence-based information, animation and a personalised dashboard to help women manage early menopause and premature ovarian insufficiency. Development of the App was undertaken as part of the CRE in Women’s Health in Reproductive Life (